
Dr. Swapan Kumar De
Senior Most Interventional Cardiologist at
Apollo Multispeciality Hospital Kolkata.
MD, DM (Cardiology)
Cardiac Device Implantation in Kolkata, India

Sometimes lifestyle changes and medication are not enough to combat heart disease. When other treatments are no longer effective, your physician may recommend an implantable cardiac device (pacemaker) to help monitor and/or regulate the rhythm of your heart. There are different types of implantable devices, and it depends on your diagnosis as to which type your doctor will choose for you. Cardiac resynchronization therapy (CRT) pacemakers help a very slow heart beat more regularly. Implantable cardioverter defibrillators (ICDs) shock the heart when it is beating too fast to prevent cardiac arrest. Additionally, some devices have been developed that can do both.
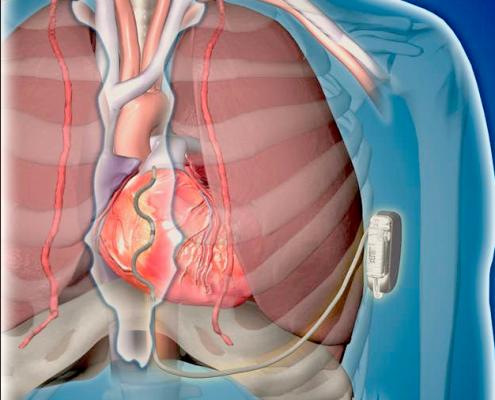
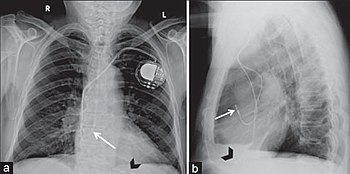
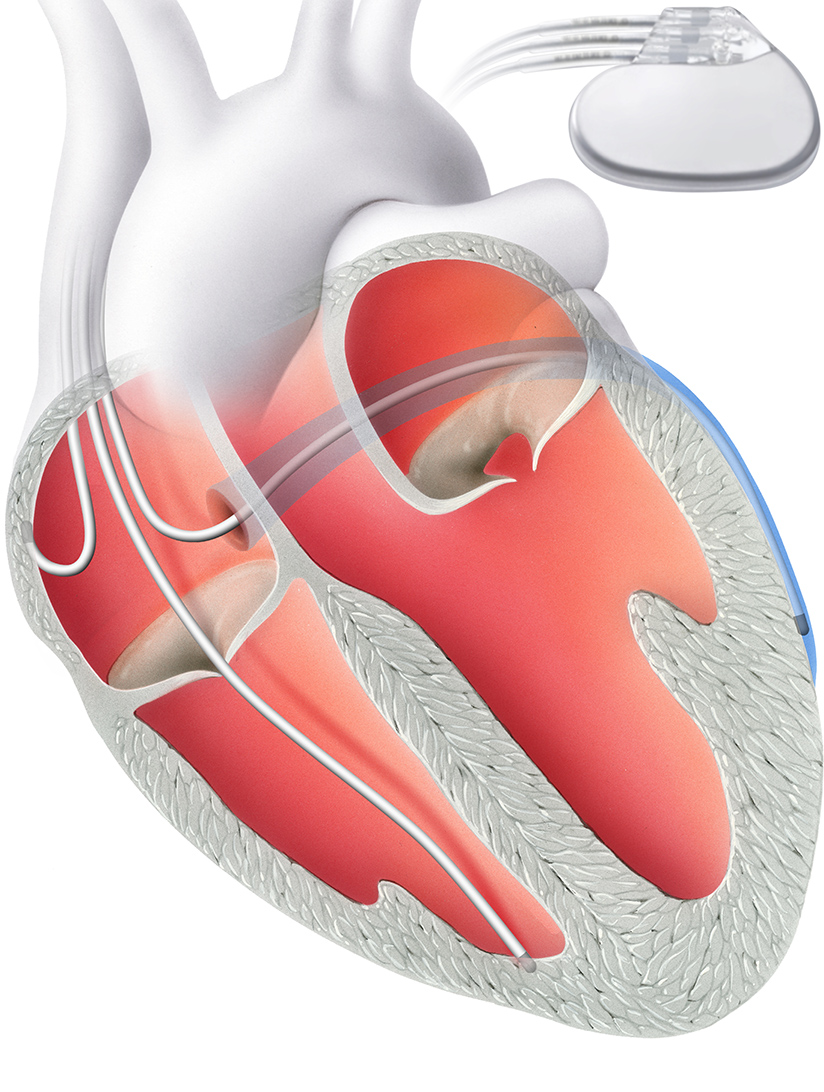
A pacemaker literally sets the pace of the heart. This tiny device is implanted under your skin and attached to your heart by tiny wires, or leads. The signals, or pacing pulses, are carried along electrical leads to the heart and stimulate the heart muscle to beat. It monitors and adjusts the heartbeat based on customized limits. If the heart rate is slower than the set low limit, an electrode sends an electrical current to the heart causing it to beat. If the heart rate is faster than the set high limit, no current is sent.
ICDs are small devices that are surgically implanted just below the collarbone. They are connected to your heart using tiny wires or leads and continuously monitor the heart's rhythm. When the heart beats to quickly, the ICD delivers a life-saving electrical current to restore the hearts normal rhythm and prevent sudden cardiac death. ICDs can also act as a pacemaker, when a slow heart rate is detected. ICDs monitor and adjust the heartbeat based on customized, high and low limits, and are similar to a pacemaker.
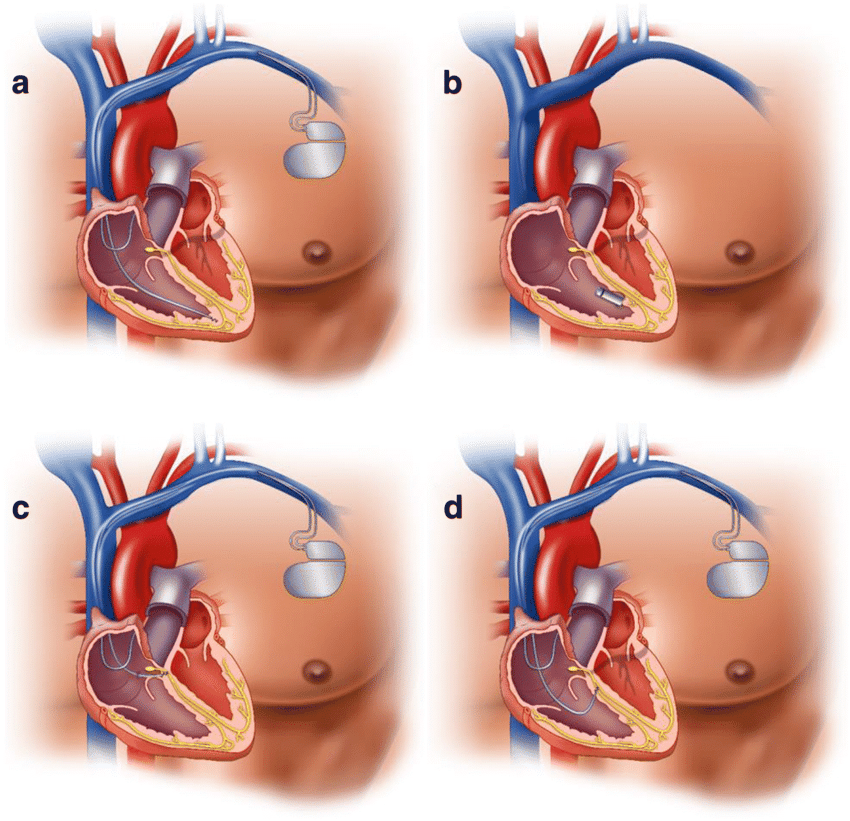
CRT is an innovative new therapy for patients with heart failure by improving the coordination of the heart's contraction. CRT builds on the technology used in pacemakers and ICDs. It also can protect the patient from slow or fast heart rhythms. The CRT device has three electrical leads that are placed in the right and left chambers of the heart - different from a pacemaker or ICD which only have electrical leads placed in the right side of the heart. This allows the CRT device to simultaneously stimulate the left and right sides of the heart and restore the heart's coordinated pumping function. This is referred to as Bi-ventricular pacing.

Types of Pacemakers
The type of pacemaker you may need depends on your symptoms and the specific heart condition you have. After our diagnostic evaluation, we discuss our recommendations with you to choose the right pacemaker for your needs.
This type of pacemaker has one lead that connects the pulse generator to one chamber of your heart.
For most people, we use the single-chamber pacemaker to control heartbeat pacing by connecting the lead to your right ventricle (lower heart chamber). Depending on your symptoms and the type of pacing you need, we connect the lead to your right atrium (upper heart chamber) to stimulate the pacing in that chamber.
With two leads, this device connects to both chambers on the right side of your heart, the right atrium and the right ventricle. The doctor programs the dual-chamber pacemaker to regulate the pace of contractions of both chambers.
This pacemaker helps the two chambers work together, contracting and relaxing in the proper rhythm. The contractions allow blood to flow properly from the right atrium into the right ventricle.
Depending on the pacing needs of your heart, a dual-chamber device may be an appropriate option for you.
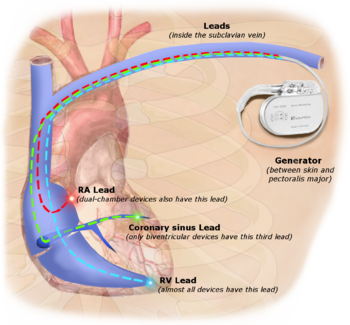
This pacemaker, also known as a cardiac resynchronization therapy (CRT) device, has three leads connected to the right atrium and both ventricles. We use the biventricular pacemaker to treat people with arrhythmias caused by advanced heart failure.
For many people with heart failure, the left and right ventricles do not pump at the same time. Our doctors program the biventricular pacemaker to coordinate the contractions of the ventricles, so that they both pump together.
Coordinating the ventricles' contractions helps your heart pump blood more efficiently and can relieve your heart failure symptoms. The treatment is known as cardiac resynchronization therapy because it resynchronizes the ventricles' pumping action.
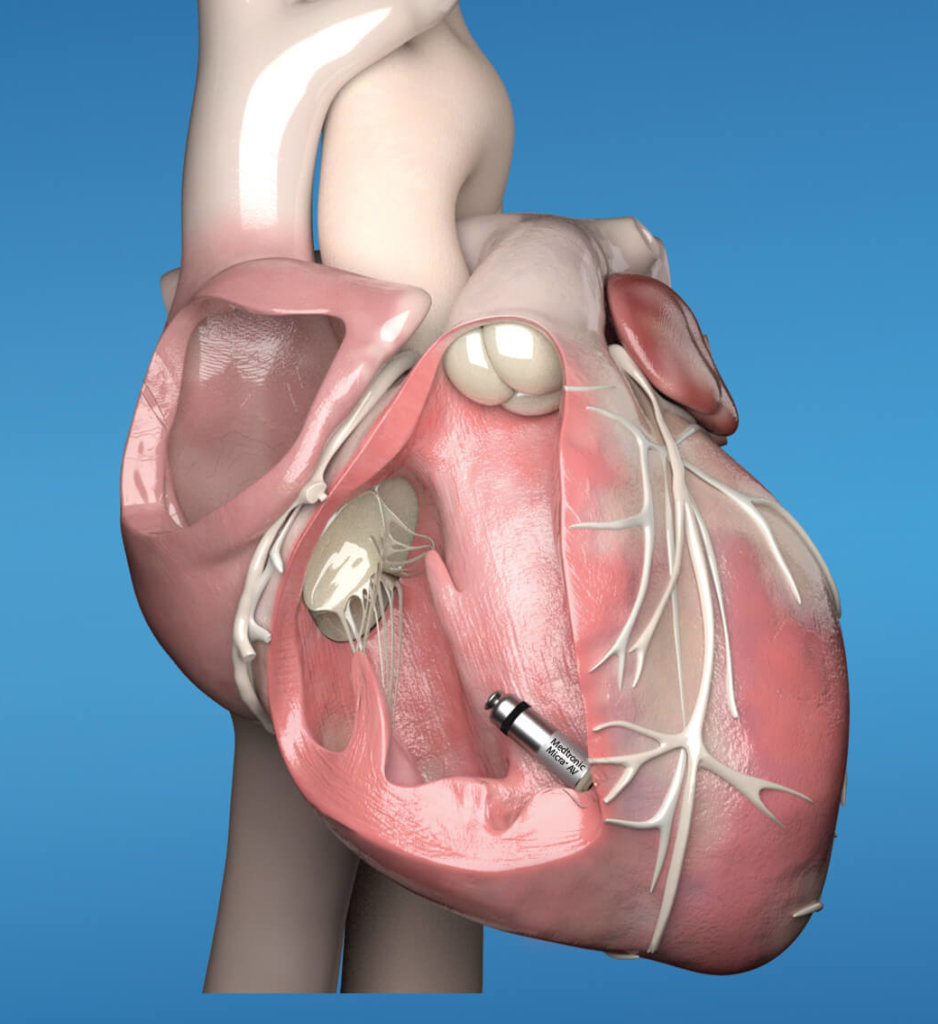
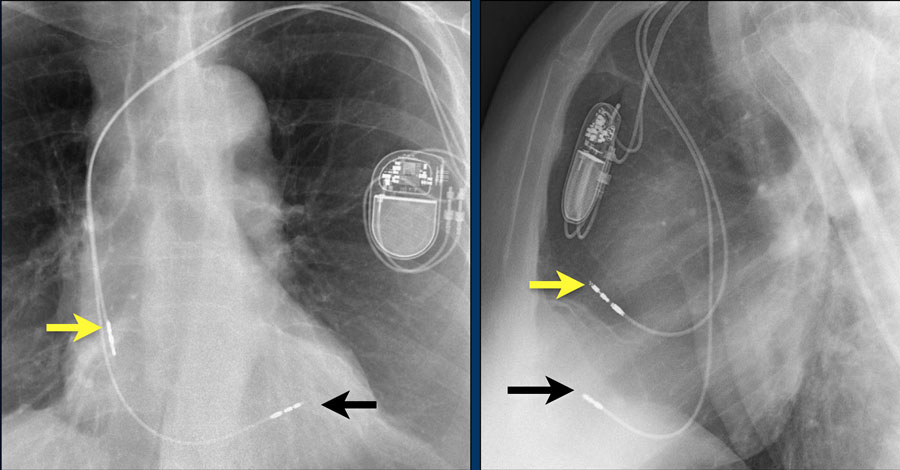
A leadless pacemaker is used to treat patients experiencing irregular or slow heartbeat (bradycardia). Like other pacemakers, the leadless pacemaker sends electrical impulses to restore the heart's rhythm and increase the heart rate.
The following are key points to remember about this review of leadless pacemakers:
1. The leadless pacemaker, which is 90% smaller than a transvenous pacemaker, is a self-contained generator and electrode system implanted directly into the right ventricle. The device is implanted via a femoral vein transcatheter approach; it requires no chest incision or subcutaneous generator pocket.
2. The primary advantage of a leadless pacemaker is the elimination of several complications associated with transvenous pacemakers and leads: pocket infections, hematoma, lead dislodgment, and lead fracture. The leadless pacemaker also has cosmetic appeal because there is no chest incision or visible pacemaker pocket.
3. Leadless pacemakers provide only single-chamber ventricular pacing and lack defibrillation capacity. Leadless pacemakers may be suitable for patients with permanent atrial fibrillation with bradycardia or bradycardia-tachycardia syndrome or those who infrequently require pacing. Leadless pacemakers are inappropriate for patients who require dual-chamber pacing, such as patients with certain forms of heart block or sinus node dysfunction.
4. Complications may occur related to femoral vein access or need for device repositioning; there is moderate risk of cardiac perforation with subsequent pericardial effusion.
5. Current leadless pacemakers are designed to be compatible with magnetic resonance imaging.
6. A leadless pacemaker is theoretically retrievable, but there is only limited experience with retrieval. Leadless pacemakers are likely to become encapsulated in cardiac tissue, as are the pacing leads of traditional pacemakers.
7. The future of leadless device technology is promising and might eventually lead to expanded pacing capabilities. One beneficial application for leadless devices may be postoperatively following transcatheter aortic valve replacement. According to one study, 28% of patients require pacemaker about 5 days after transcatheter aortic valve replacement.
* Consult your physician if you have any questions about pacemakers or heart disease.
About Cardiologists : Cardiologists treat people with diseases or conditions of the heart and people who want to learn the risk factors for heart disease. A primary care doctor or family practice doctor can work with a cardiology specialist to diagnose, treat, and manage heart conditions and help people make heart-healthy lifestyle choices. Patients who are at risk for heart disease or have a history of heart symptoms may see a clinical cardiologist regularly. People with ongoing heart conditions, pacemakers, or frequent heart trouble are likely to see a cardiologist with a subspecialty.